%20(960%20x%20540%20px)%20(1200%20x%20630%20px)%20(1600%20x%20900%20px)%20(1600%20x%20900%20px)%20(98).png?width=1130&height=636&name=Untitled%20(560%20x%20420%20px)%20(960%20x%20540%20px)%20(1200%20x%20630%20px)%20(1600%20x%20900%20px)%20(1600%20x%20900%20px)%20(98).png)
Restless Legs Syndrome in Menopause: What Every Woman Should Know
This lesson will help you understand what RLS is, why it worsens during menopause, and what evidence-based strategies exist to manage it.
🔍 1. What is Restless Legs Syndrome (RLS)?
RLS is a neurological condition that causes an irresistible urge to move the legs, often accompanied by tingling, crawling, or pulling sensations—like someone is gently tickling up and down your leg... but won’t stop.
-
Worse at night: Symptoms typically peak in the evening or when lying down.
-
Leads to sleep disruption: Many women struggle to fall or stay asleep due to these symptoms.
📈 2. RLS and Menopause: Why It Matters
RLS is more common in women, and prevalence increases with age—particularly during the menopausal transition.
-
Perimenopause: RLS symptoms often worsen, especially in women with hot flashes or night sweats.
-
Postmenopause: The highest RLS rates are reported here, with up to 16% affected—and some studies show RLS may be linked to 63.8% of sleep disorders in this group.
⚠️ Why RLS Gets Worse in Menopause:
-
Hormone Changes: Declining estrogen and progesterone disrupt dopamine (a key neurotransmitter in RLS).
-
Iron Deficiency: Common in midlife and strongly associated with RLS severity.
-
Sleep Issues: Hot flashes and insomnia amplify symptoms.
💢 3. Symptom Severity & Risk Factors
-
69% of women report RLS gets worse after menopause.
-
Higher risk if you have:
-
Low iron/ferritin (<50 ng/mL)
-
Hypertension, diabetes, anemia
-
Higher BMI or lower income
-
Smoking or alcohol use
-
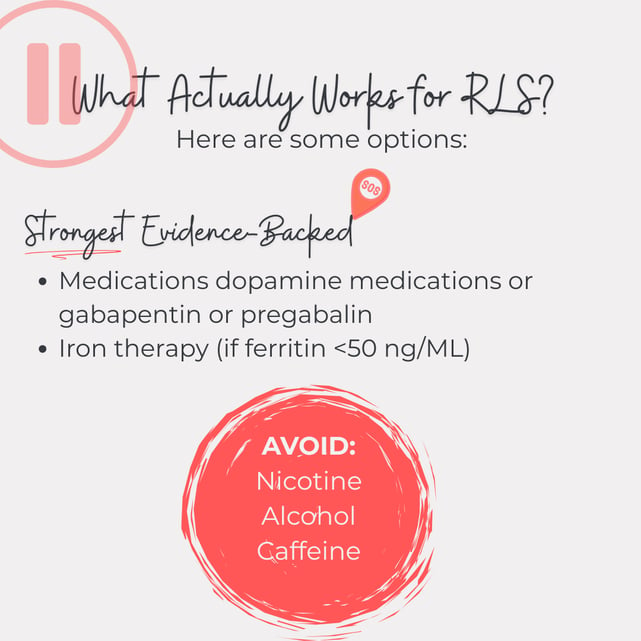
✅ 4. Relief Strategies & Treatments
🧘♀️ Lifestyle & Non-Drug Approaches
-
Movement: Stretching, walking, or gentle yoga may relieve symptoms.
-
Hot/cold therapy: Alternating baths or compresses can help.
-
Sleep hygiene: Consistent sleep schedule, limit screen time, cool sleeping environment.
-
Avoid triggers: Reduce caffeine, alcohol, nicotine.
-
Mental distractions: Reading, puzzles, or mindfulness exercises.
💊 Medical Treatments
-
Iron supplementation (only if ferritin <50 ng/mL).
-
Dopamine agonists (e.g., pramipexole, ropinirole).
-
Gabapentin or pregabalin, especially if pain is involved.
-
Opioids: Reserved for severe, treatment-resistant cases under specialist care.
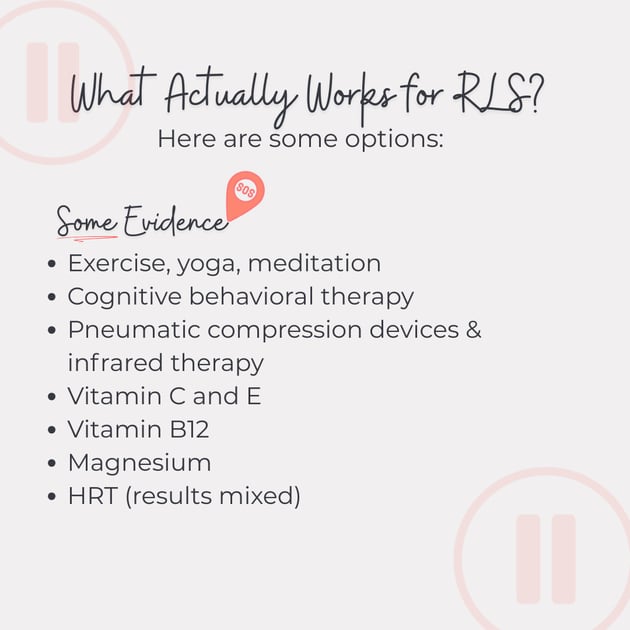
🌿 5. Supplements & Adjuncts
-
Vitamin C & E: Antioxidant support—some studies show reduced RLS severity.
-
Magnesium: Some evidence supports use (especially magnesium oxide/citrate).
-
Vitamin B12: Lower levels linked to worse symptoms, but more research is needed.
🔄 6. HRT—Helpful or Not?
-
Mixed evidence: Not a primary treatment for RLS.
-
May help indirectly by improving sleep or vasomotor symptoms.
-
Some women report worsening—monitor closely if starting HRT.
🛠️ 7. Other Non-Pharmacological Therapies
-
Exercise, yoga, meditation
-
Pneumatic compression devices
-
Infrared light therapy
-
Cognitive Behavioral Therapy (CBT)
-
Acupuncture or light therapy (promising but early research)
Here is a breakdown based on level of evidence:
💡 8. Key Takeaways
-
RLS is more than annoying—it disrupts sleep, energy, and quality of life.
-
Menopausal hormone shifts and iron deficiency play a big role.
-
A combined approach of lifestyle, medical treatment, and targeted supplementation offers the best outcomes.
Want to Read More?
Wesström, J., Nilsson, S., Sundström-Poromaa, I., & Ulfberg, J. (2008). Restless legs syndrome among women: prevalence, co-morbidity and possible relationship to menopause. Climacteric, 11, 422 - 428. https://doi.org/10.1080/13697130802359683.
Bagheri, R., Abedi, P., Mousavi, P., & Azimi, N. (2018). The prevalence of restless legs syndrome and its relationship with demographic characteristics and medical disorders in postmenopausal Iranian women. Health Care for Women International, 39, 1317 - 1325. https://doi.org/10.1080/07399332.2018.1435662.
Bhuvaneshwari et al. "A study to assess the knowledge on restless legs syndrome among perimenopausal women." International Journal of Nursing and Health Sciences (2020). https://doi.org/10.33545/26649187.2020.v2.i1a.19.
M. Siemiński et al. "Restless Legs Syndrome and Hormonal Replacement Therapy in Women at Menopausal Age (P05.010)." Neurology, 78 (2012). https://doi.org/10.1212/WNL.78.1_MEETINGABSTRACTS.P05.010.
N. Salari et al. "Global prevalence of sleep disorders during menopause: a meta-analysis." Sleep & Breathing = Schlaf & Atmung (2023): 1 - 15. https://doi.org/10.1007/s11325-023-02793-5.
C. Comella et al. "Treatment of Restless Legs Syndrome." Neurotherapeutics, 11 (2013): 177 - 187. https://doi.org/10.1007/s13311-013-0247-9.
M. Seeman et al. "Why Are Women Prone to Restless Legs Syndrome?." International Journal of Environmental Research and Public Health, 17 (2020). https://doi.org/10.3390/ijerph17010368.
J. Winkelman et al. "Practice guideline summary: Treatment of restless legs syndrome in adults." Neurology, 87 (2016): 2585 - 2593. https://doi.org/10.1212/WNL.0000000000003388.
Xiao-min Xu et al. "Complementary and alternative therapies for restless legs syndrome: An evidence-based systematic review.." Sleep medicine reviews, 38 (2017): 158-167 . https://doi.org/10.1016/j.smrv.2017.06.003.
Eloise G Harrison et al. "Non-pharmacological interventions for restless legs syndrome: a systematic review of randomised controlled trials." Disability and Rehabilitation, 41 (2019): 2006 - 2014. https://doi.org/10.1080/09638288.2018.1453875.
H. Attarian et al. "Treatment of chronic insomnia disorder in menopause: evaluation of literature." Menopause, 22 (2015): 674–684. https://doi.org/10.1097/GME.0000000000000348.
N. Marshall et al. "Magnesium supplementation for the treatment of restless legs syndrome and periodic limb movement disorder: A systematic review.." Sleep medicine reviews, 48 (2019): 101218 . https://doi.org/10.1016/j.smrv.2019.101218.
Pedro González-Parejo et al. "Effects of Dietary Supplementation in Patients with Restless Legs Syndrome: A Systematic Review." Nutrients, 16 (2024). https://doi.org/10.3390/nu16142315.
S. Gorantla et al. "Magnesium citrate monotherapy improves RLS symptoms and multiple suggested immobilization test scores in an open-label pilot study.." Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine (2024). https://doi.org/10.5664/jcsm.11206.
Chaofan Geng et al. "Possible association between vitamin B12 deficiency and restless legs syndrome." Clinical Neurology and Neurosurgery, 223 (2022). https://doi.org/10.1016/j.clineuro.2022.107477.
D. Kennedy et al. "B Vitamins and the Brain: Mechanisms, Dose and Efficacy—A Review." Nutrients, 8 (2016). https://doi.org/10.3390/nu8020068.
M. Sagheb et al. "Efficacy of vitamins C, E, and their combination for treatment of restless legs syndrome in hemodialysis patients: a randomized, double-blind, placebo-controlled trial.." Sleep medicine, 13 5 (2012): 542-5 . https://doi.org/10.1016/j.sleep.2011.11.010.
Pedro González-Parejo et al. "Effects of Dietary Supplementation in Patients with Restless Legs Syndrome: A Systematic Review." Nutrients, 16 (2024). https://doi.org/10.3390/nu16142315.
Giorgos K. Sakkas et al. "Current trends in the management of uremic restless legs syndrome: a systematic review on aspects related to quality of life, cardiovascular mortality and survival.." Sleep medicine reviews, 21 (2015): 39-49 . https://doi.org/10.1016/j.smrv.2014.07.006.
.png?width=50&name=Take%20control%20over%20(13).png)
%20(960%20x%20540%20px)%20(1200%20x%20630%20px)%20(1600%20x%20900%20px)%20(1600%20x%20900%20px)%20(85)-1.png?width=352&name=Untitled%20(560%20x%20420%20px)%20(960%20x%20540%20px)%20(1200%20x%20630%20px)%20(1600%20x%20900%20px)%20(1600%20x%20900%20px)%20(85)-1.png)


