Building Bones of Steel
The Ultimate Guide to Optimal Bone Health

Of the estimated 10 million Americans with osteoporosis, about 80% are women.
- An additional 27.3 million women have osteopenia a precursor to osteoporosis.
- Approximately one in two women over age 50 will break a bone because of osteoporosis.
Osteoporosis is called the “silent disease” because until a bone is broken, people are generally unaware they have it. Osteoporosis is the main cause of fractures in postmenopausal women (average age 55+).
Osteoporosis is a systemic skeletal disease characterized by low bone mass and structural deterioration of bone tissue, leading to bone fragility and an increased risk of fracture. Women have a greater lifetime fracture risk (40%) than men (13%) due to their typically smaller, thinner bones.
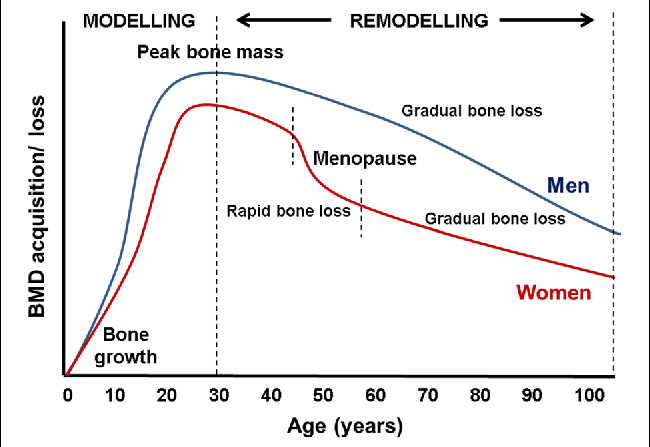
Women also tend to lose bone at a younger age and at a quicker pace than men (4). Additionally, estrogen plays a critical role in bone development, and it begins declining as women enter perimenopause, creating a significantly higher risk for osteoporosis in postmenopause.
Decrease in bone density is particularly fast in the 5-10 years around the menopause transition due to loss of the protective effect of estrogen. During that rapid bone loss, the delicate structure (microarchitecture) of the skeleton is damaged, weakening the bone and predisposing to a fracture (a “bone attack”). This is the critical window to protect bones.
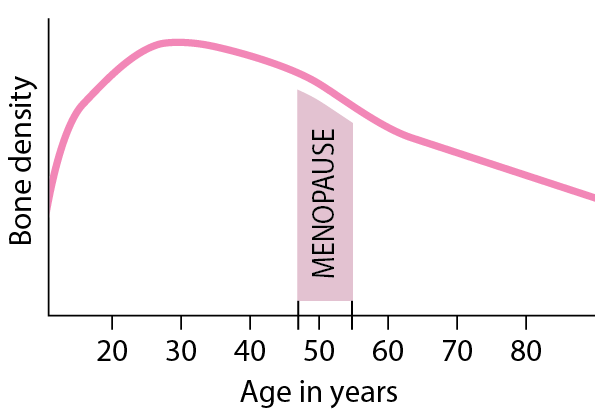
This means that we must begin taking our bone health seriously in perimenopause (or before).
Your state of health as you enter into menopause correlates with your health and longevity postmenopause. It is the last chance you have to enhance bone health or to reverse any damage. You can minimize future damage but not restore back without pharmacologic intervention.
A risk assessment and potential bone density scan (DEXA) can identify bone health and potential problem areas.
If conducted prior to menopause, preventative steps can be taken to improve bone mass in advance of menopause when bone deteriorates at an accelerated rate. A DEXA can also reveal information about muscle composition and fat mass. Therefore, it provides the same opportunity for enhancing lean muscle mass prior to estrogen decline.
Currently, DEXA scanning rates are low even among women within the recommended guidelines.
Current medical guidelines advise physicians to consider a DEXA scan for women over 65 at moderate risk, only advising it for a younger demographic (50 to 69) if there are risk factors for severe bone loss (1,7,8).
The Society for Women’s Health Research (SWHR) convened an expert review of these clinical guidelines.
- It concluded that given rapid bone loss can occur in women during early postmenopausal years, leading to increased risk for osteoporosis, there is a missed opportunity for health promotion and prevention by not focusing on bone health during perimenopause rather than until after 65 (well into postmenopause).
- The average age of menopause in North America is 51 years old (range 45 to 55 years). Waiting to engage women more than 10 years postmenopause means they cannot introduce preventive lifestyle practices and potential treatment options that may preserve bone density and reduce fall and fracture risk.
In fact, the Working Group concluded that the guidelines should reduce the age for screening to perimenopause (ages 40-50) to provide a baseline assessment of bone health before the majority of rapid postmenopausal bone loss has already occurred. This baseline can be used to monitor changes throughout the menopause transition (8).
A study of data from 2008 to 2014 found overall screening rates were: 21.1%, 26.5%, and 12.8% among women ages 50–64, 65–79, and 80+ years, respectively. Even after fracture, very few providers screen, meaning women need to self-advocate and raise the issue themselves with their physicians (6).